Every morning, I receive two messages from my parents—not greetings, not updates, but their blood pressure readings. Both are on regular medication. It’s their way of managing their health—and maybe, in their quiet way, of asking, “Are we still being cared for?”
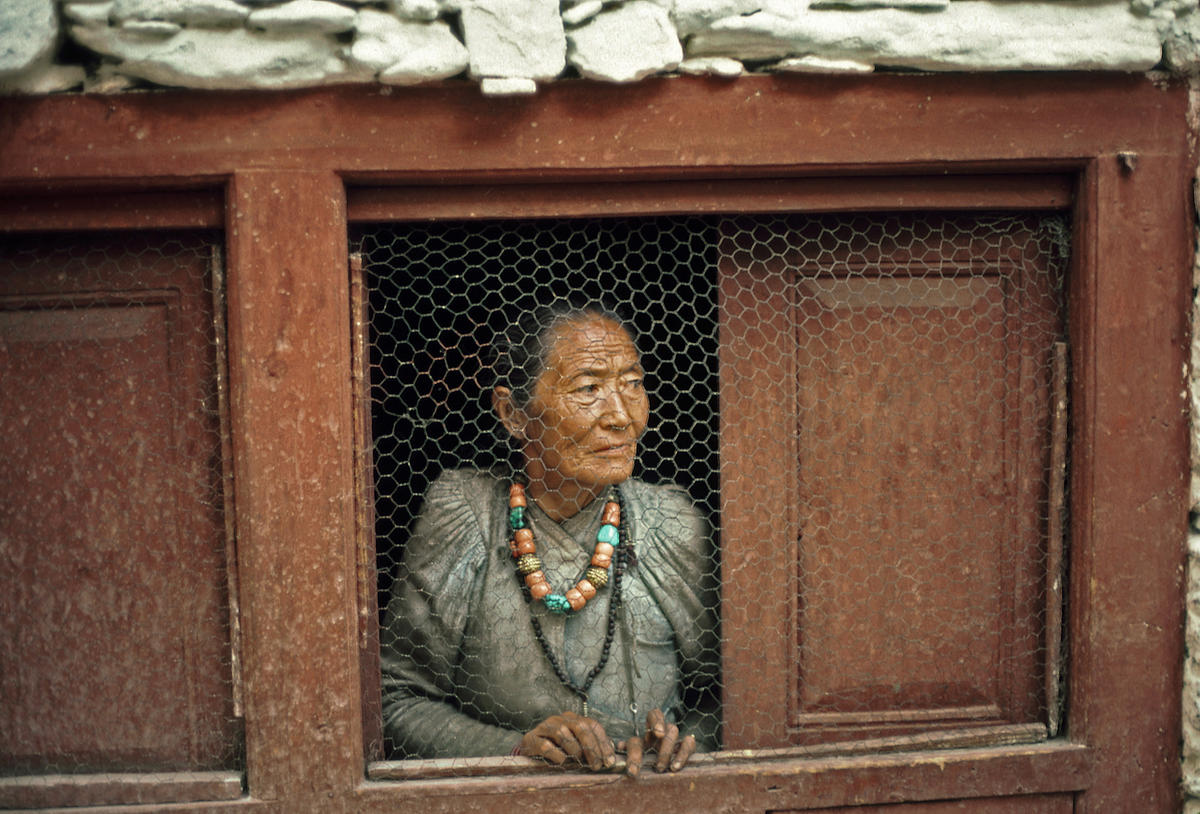
That simple gesture says more than words ever could. Across Nepal, a generation is ageing with dignity, even as the systems meant to support them fall dangerously behind.
The Silent Surge of Ageing
Nepal is ageing. Fast. The World Health Organization (WHO) estimates that by 2030, people aged 60 and above will make up over 15% of our population—nearly double today’s figure. By 2050, one in every four Nepalese will be elderly (WHO SEARO, 2022).
These aren’t just numbers. They are our parents, neighbors, teachers, and local leaders—the people who built the foundation we now stand on.
This demographic shift has been called a “silent revolution.” In Nepal’s case, it’s a revolution we’ve barely begun to prepare for.
When the Family System Fades
Traditionally, elders were the heart of Nepali households. However, times have changed. Migration, urbanization, and shifting family dynamics have disrupted that support system. Many elderly now live alone—especially in rural areas—while their children work abroad or in distant cities.
Social isolation and loneliness, according to WHO’s Decade of Healthy Ageing report, are among the top threats to elderly wellbeing, with real impacts on both mental and physical health.
Even families that want to help struggle to balance jobs, finances, and time. The safety net that once cushioned our elders is wearing dangerously thin.
A Health System Not Built for Ageing
With age comes a heavier burden of non-communicable diseases. Globally, over 70% of older adults live with at least one chronic illness like diabetes, hypertension, or arthritis (WHO Global Health Estimates, 2023). Nepal is no exception.
Yet our health system is still focused on short-term, acute care. We have fewer than a dozen geriatricians nationwide. Most hospitals lack elder-friendly design. Primary care workers are rarely trained to handle memory loss, mental health issues, or mobility concerns.
WHO’s Age-friendly Primary Health Care Guidelines recommend regular check-ups, counselling, and outreach—but in many parts of Nepal, elders walk hours to reach health posts, only to return without treatment.
Loneliness: The Invisible Illness
Perhaps the most devastating—and most overlooked—aspect of ageing is loneliness.
The WHO has formally declared loneliness a public health concern, linking it to depression, dementia, and early death. In Nepal, especially in semi-urban and rural communities, older adults wait for calls from their children working abroad, attend fewer community events, and often go days without meaningful conversation. This invisible suffering needs urgent recognition—and should be addressed.
Time for a National Commitment
We must stop treating elder care as a private, family matter. It’s time to act—together.
Here’s what Nepal needs now:
A National Elder Care Strategy
A comprehensive, cross-sectoral plan for long-term care, home support, social security, and legal protections. Culturally rooted jestha sewa and sneha kendras (elder care and compassion centers) should become part of every community.
A Trained, Compassionate Health Workforce
Geriatric care must be included in MBBS and nursing courses—with modules on ageing, mental health, traditional healing, and end-of-life care. Our health workers must be trained not only to treat, but also to listen.
Elder-Friendly Communities
Our public spaces should be safe and welcoming. Benches under trees, handrails near temples, ramps at ward offices, and “senior corners” in health facilities with dignity and priority seating.
Intergenerational Connections
Let’s bridge generations. School children can visit old age homes. Youth can document oral histories. Traditional guthis and tole sabhas can be revived to include the care of the elderly as part of their mandate.
Technology with Heart
From FM radio shows sharing elderly stories to community volunteers teaching phone use, tech can be a lifeline. Imagine a “Call-a-Bajai/Bajey” program, where weekly check-ins bring not just health reminders but warmth.
Inclusion in Local Governance
Elders should be part of community planning, disaster preparedness, and cultural preservation. They’re not just dependents—they’re knowledge-keepers.
In Conclusion: Let’s Turn Reverence into Action
Ageing is not a burden—it’s a blessing. Longer lives mean healthier lives. But living longer must come with living well.
Nepali culture teaches us to bow down and to honor them as buwa and aama even if they are strangers. But that reverence must go beyond rituals.
Let us match our respect with real action—through policy, healthcare, community support, and human connection.
In caring for our elders, we honor our past.
In preparing for their needs, we safeguard our future.
Dr. Kishori Mahat is a public health specialist.
Dr. Kishori Mahat
Published: July 6, 2025